International Journal of Cardiovascular Sciences. 29/maio/2025;38:e20240210.
Cardiac Autonomic Neuropathy: An Emerging Cardiovascular Risk to Hemodialysis and Non-Hemodialysis Chronic Kidney Disease Patients of Primary Renal Diagnosis
Abstract
Background:
Patients with chronic kidney disease (CKD) are at higher risk of cardiovascular disease. A dysfunctional autonomic nervous system may be the underlying cause. However, very few studies have determined the status of cardiac autonomic neuropathy (CAN) in both non-hemodialysis and hemodialysis CKD patients.
Objectives:
The present study intended to determine and compare CAN in both non-hemodialysis and hemodialysis CKD patients of primary renal diagnosis only and its correlation with the progression of the disease.
Methods:
Non-hemodialysis and hemodialysis CKD patients (n = 23 in each group) of both sexes of 18 to 50 years were recruited in this cross-sectional, observational study. Resting blood pressure and heart rate (HR) were measured, and lead II ECG was recorded for analysis of time- and frequency-domain measures of heart rate variability (HRV). Mann-Whitney U test was applied to compare the variables between the two groups. Spearman correlation was conducted to examine the relationship between variables and the stage of the disease (non-hemodialysis and hemodialysis CKD). A 2-tailed p value < 0.05 was taken as the cutoff level of significance.
Results:
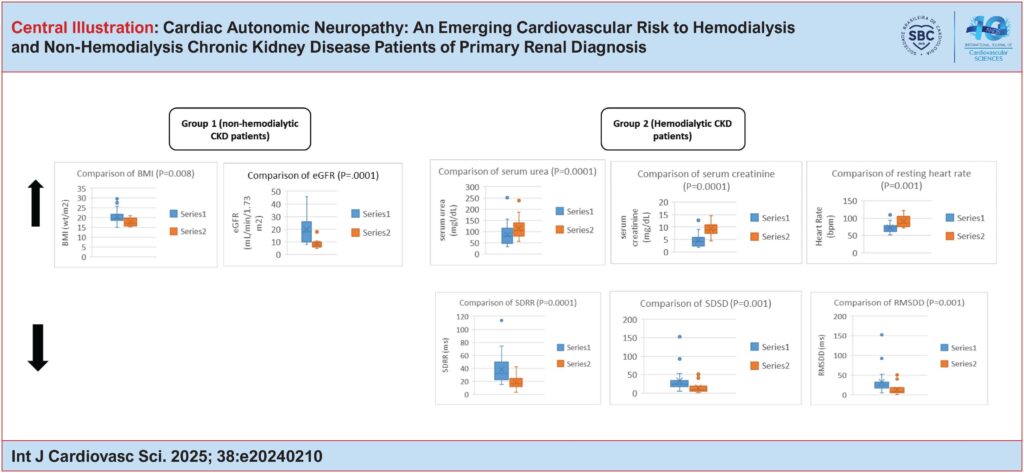
Body mass index (BMI) was significantly higher in non-hemodialysis patients (p = 0.008). Resting HR was significantly higher in the hemodialysis group (p = 0.001). Among HRV measures, standard deviation of RR intervals (SDRR; p = 0.0001), standard deviation of successive differences (SDSD; p = 0.001), and root mean square of successive RR intervals (RMSSD; p = 0.001) were significantly lower in the hemodialysis group. Peripheral blood pressure was not significantly different between the two groups. Resting HR (r = 0.498, p = 0.001) was positively associated with the end-stage renal disease. However, SDRR (r = −0.507, p = 0.001), RMSSD (r = −0.507, p = 0.001), and BMI (r = −0.427, p = 0.004) were negatively associated with end-stage renal disease.
Conclusion:
Altered autonomic function was more profound in hemodialysis patients as evidenced by increased resting HR and decreased HRV measures (SDRR, SDSD, and RMSSD). Moreover, altered autonomic function was associated with end-stage renal disease. Therefore, CKD patients may be screened for CAN for early detection of cardiovascular disease.
334