International Journal of Cardiovascular Sciences. 29/Sep/2020;33(5):586-8.
Potential Role of Hematological Parameters in Patients with Acute Myocardial Infarction: viewpoint
Graphical Abstract
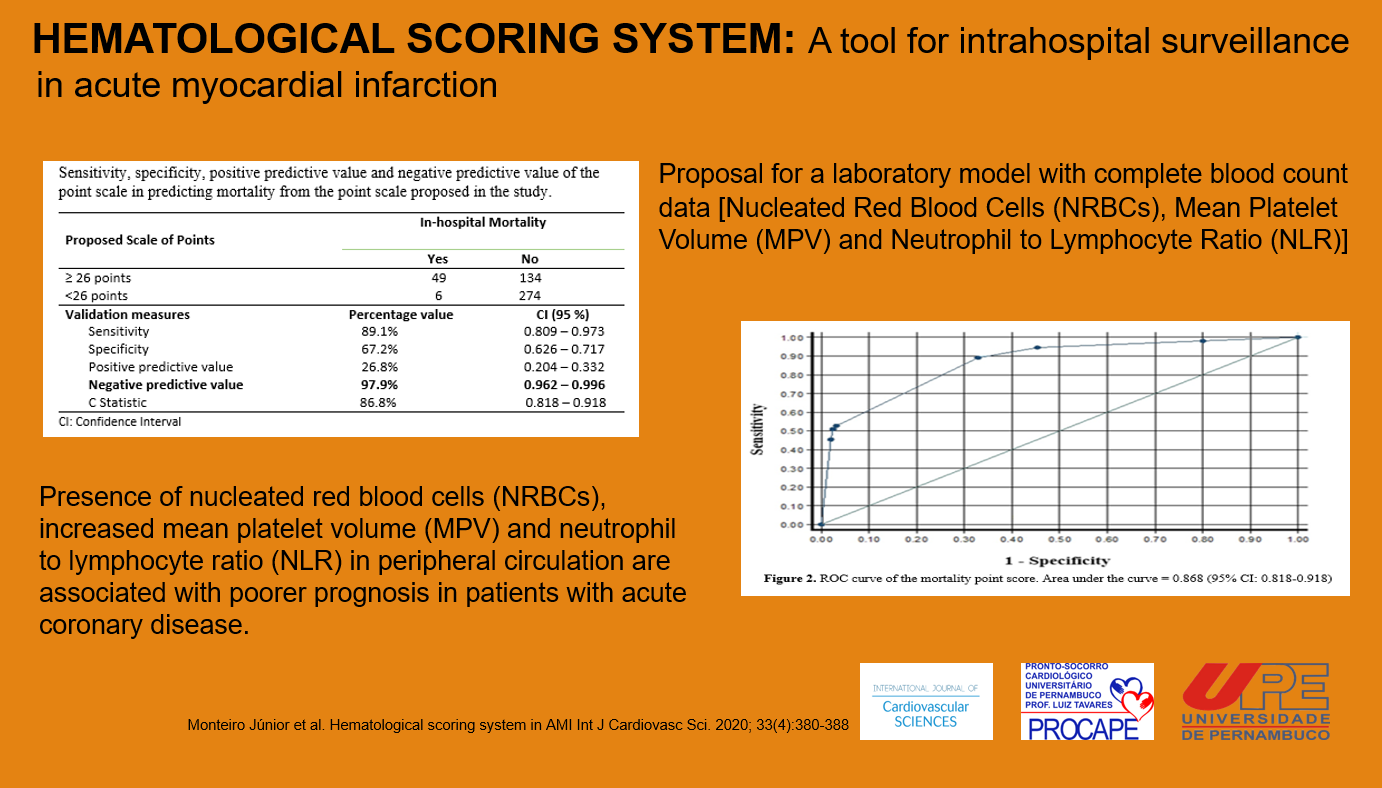
Acute myocardial infarction (AMI) is one of the most important cardiovascular diseases, leading to disability and death worldwide. Atherosclerosis is the main etiology of AMI, which is characterized by a series of highly specific cellular and molecular responses that can best be described, in aggregate, as an inflammatory disease. Risk factors such as arterial hypertension, diabetes mellitus, smoking, dyslipidemia, obesity, emotional stress and family history are not, in themselves, sufficient for in-hospital risk assessment of patients with AMI. Recently, several studies have found an association between oxidative stress, due to inflammation, and hypoxemia processes, with hematological changes and coronary arterial diseases, suggesting their usefulness in identifying the risk of death. These studies have shown the association of hematological parameters with prognostic biomarkers in patients with coronary artery disease. – This issue of the International Journal of Cardiovascular Sciences includes the paper “Performance of a Hematological Scoring System in Predicting All-Cause Mortality in Patients with Acute Myocardial Infarction”, with a proposed scoring system for in-hospital surveillance.
Several studies have shown that hypoxemia and infection are the main stimulus to differentiation processes in distinct hematological cell lines in the bone marrow, when hematological diseases, cancer, congestive heart failure, acute and chronic anemias are excluded. , These cells originate from a single progenitor cell called the stem cell, when for example, blood exposure to low oxygen concentrations over a long period results in differentiation and increased production of red blood cells. This stimulus to the bone marrow is produced by erythropoietin, a glycoprotein, 90% of which is produced in the kidneys, the rest being mostly formed in the liver, in response to hypoxemia. Infectious diseases cause the differentiation and final formation of specific types of leukocytes for each pathogen. Platelets have an important role in hemostasis, inflammation and innate immunity. In the last five decades, with the advent of automated counting, the hemogram was transformed into a useful clinical tool to demonstrate the daily variability in the hematopoietic response according to the patient’s injury. , In recent years, a large number of studies have provided a better knowledge of these hematological parameters, with independent information on pathophysiology and risk stratification. For example, nucleated red blood cells (NRBCs) are immature erythrocyte cells present in the bone marrow in the process of hematopoiesis. In a healthy adult, there are no NRBCs in the peripheral blood. Therefore, the presence of NRBCs in the peripheral circulation is associated with a poorer prognosis. – The neutrophil to lymphocyte ratio (NLR), a combination of two independent markers of inflammation, is considered a simple and nonspecific marker of inflammation. White blood cells, particularly lymphocytes, cause a major important modulation in the inflammatory response. Clinical and experimental studies have associated lymphopenia with progressive atherosclerosis. , Basem et al., demonstrated that NLR is a strong predictor of short- and long-term mortality in stable and unstable coronary insufficiency. Patients with non-ST-segment elevation myocardial infarction with NLR > 4.7 have a mortality rate of 29.8%, whereas those with NLR < 3 have a mortality rate of 8.4 (p <0.001). In another study, using a 2.54 cut-off point, NLR was a predictor of severe atherosclerosis, with a sensitivity of 74% and specificity of 53% (ROC curve 0.627; 95% CI: 0.545-0.704, p = 0.004). There are also studies demonstrating the association between NLR and the extent and severity of coronary artery disease. , Large platelets are metabolically and enzymatically more active than small platelets and are characterized by an elevation in mean platelet volume (MPV). In the study by Uysal et al., an MPV value greater than 10.4 is considered a predictor of severe atherosclerosis, with a senstitivity of 39% and specificity of 90% (ROC curve: 0.631, 95% CI: 0.549-0.708, p = 0.003), and can be used as a predictor and cardiac risk identifier in patients with coronary artery disease. MPV has thus been identified as an independent risk factor for acute myocardial infarction in patients with coronary artery disease. ,
[…]
2,424